
Hormonal (regular dose - 52mg) IUD
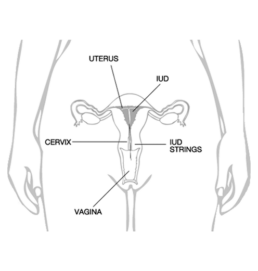
The hormonal (regular) IUD is a small, T-shaped device that is inserted into the uterus to provide long-acting reversible contraception. It is made of soft, flexible plastic and is designed to prevent pregnancy by releasing a low dose (52mg) of the hormone levonorgestrel directly into the uterus.

Hormonal (lower dose - 19.5mg) IUD
A hormonal lower dose IUD is a hormonal intrauterine device (IUD) that is used for long-term birth control. It is a small, T-shaped device that is inserted into the uterus by a healthcare professional. The IUD releases a hormone called levonorgestrel (at the lowest dose of 19.5mg), which helps prevent pregnancy.

Both devices are licensed for contraceptive use up to 5 Year duration.
What are the differences between the two hormonal IUD's?
The hormonal IUD (regular dose of 52mg of Levonorgestrel) is licensed for three main indications for use: 1) contraception, 2) menstrual control and 3) the progestogen component of Menopausal Hormonal Therapy (Hormone Replacement Therapy). It is particularly suited to women who have heavy periods or menstrual problems and those who may be approaching pre menopause. It can be used off-license for 7 years of contraception if inserted after the age of 45Y.
The other hormonal IUD (lower dose of 19.5mg of levonorgestrel) is licensed for contraception only and has a smaller frame and insertion cannula compared to the regular dose hormonal IUD. This makes it particularly suited to younger women, women with a small uterus and those who have never had a child. Its lower hormonal dose means that it may not suppress periods as successfully as the regular dose hormonal IUD, but women may also experience less hormonal side effects including less risk of benign ovarian cysts with the lower dose system.
Advantages of hormonal IUDs
- Long acting – they last for 5 years
- Highly effective contraception (>99%)
- Cost effective over the 5-year period
- Low incidence of hormonal side effects in most women because the hormone tends to work more locally in the uterus as there is minimal absorption systemically.
- Lightens periods and many women may stop having periods altogether and this is very safe. In fact, it reduces uterine cancer and possibly ovarian cancer.
- Reduced bleeding often leads to reduced period pain
- Rapid return to fertility once the device is removed
Disadvantages of hormonal IUDs
- Does not protect against STIs. A condom would be best placed to prevent sexually transmitted infections
- Some women may develop hormonal side effects, eg. acne, bloating, headaches, weight gain, weight loss
- The regular dose 52mg hormonal IUD may increase risk of benign ovarian cysts, whereas the lower dose 19.5mg has less risk of benign ovarian cysts
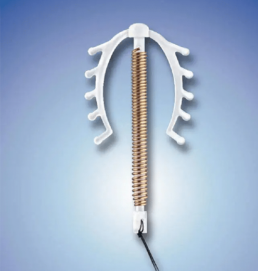
Copper IUD (Non Hormonal)
The Copper IUD is designed to be effective for an extended period, typically ranging from five to ten years, depending on the specific model. It provides long-term contraception without requiring daily attention or regular maintenance. The device is inserted into the uterus by a healthcare professional during an office visit.
Once inserted, the Copper IUD works primarily by preventing fertilisation but can also interfere with the implantation of an egg in the uterus. It does not protect against sexually transmitted infections (STIs) and is solely intended for contraception purposes.
While the Copper IUD offers long-term effectiveness and convenience, it may cause certain side effects for some individuals. These can include irregular bleeding, increased menstrual cramping, and changes in menstrual flow. It is essential to consult with a healthcare provider to determine if the Copper IUD is suitable for your specific needs and medical history.
Benefits of Non Hormonal IUD's
Non-hormonal intrauterine devices (IUDs) offer several benefits as a form of contraception. Some of the advantages of non-hormonal IUDs include:
Highly effective: Non-hormonal IUDs are one of the most effective forms of contraception available. They have a very low failure rate, with a failure rate of less than 1%. Once inserted correctly, they provide long-term contraception without requiring daily attention or user compliance.
Non-hormonal: Unlike hormonal contraceptive methods, non-hormonal IUDs do not release any hormones into the body. This can be appealing for individuals who prefer to avoid hormonal contraception or those who may have contraindications or concerns related to hormonal methods.
Long-lasting: Non-hormonal IUDs are designed to provide contraception for an extended period, typically ranging from 5 to 10 years, depending on the specific model. This makes them a convenient option for individuals who desire long-term contraception without the need for frequent replacements.
Rapid return to fertility: Once a non-hormonal IUD is removed, fertility typically returns quickly. Unlike some hormonal methods that may require a longer period for the body to adjust and regain normal fertility, non-hormonal IUDs do not have a significant impact on the menstrual cycle or ovulation.
Suitable for breastfeeding: Non-hormonal IUDs are considered safe for use while breastfeeding. They do not affect breast milk production or quality, and the copper ions released by the IUD are not transmitted to the breast milk or the baby.
Non-interfering with sexual spontaneity: Once the non-hormonal IUD is inserted, it does not require any further action during sexual activity. There is no need to interrupt intimacy for contraceptive purposes or remember to take a contraceptive pill or use barrier methods before each act of intercourse.
Sedation with IUD
At GCA, we insert all IUDs under intravenous sedation, to eliminate pain and discomfort during the insertion process.
If you prefer to be awake, then many GPs can insert the IUDs in their offices.
Sometimes the GP may have difficulty inserting an IUD, when you are awake. If this has happened to you, then we recommend attempting the insertion under sedation.
Risks of IUD insertions include pain, infection, perforation, or expulsion of the device. You will be counselled through these issues in detail when you attend for your IUD insertion, where you will be required to sign a consent form.
How to make a booking for consultation and insertion of an IUD under sedation?
- They are best inserted within 7 days of the period starting (but that timing may not always be possible). Day 1 = first day of period. Therefore, insertion may be any time from day 1 to day 7.
- If a non-expired IUD is already in place, and you need it replaced, you may book at any time
- If a non-expired contraceptive implant is still in your arm, then the IUD may be inserted at any time
- If you are taking the oral contraceptive pill and no missed pills, and no more than 7 days of sugar (dummy) pills, then IUD may be inserted.
- Abstinence (no sex at all) from intercourse for 3 weeks is required before insertion, if less effective (eg. condoms) or no contraception is being used, or you have an expired IUD or expired implant in the arm.
- If you have recently had a baby (> 8 weeks ago) and are fully breastfeeding and you have not had intercourse yet, then insertion may take place.
- You must have a BMI <40 to be eligible to have sedation at the clinic. This is a safety issue for any type of sedation or anaesthesia.
- We don’t stock the IUDs and they must be brought with you. A prescription from your GP is necessary to acquire any type of IUD from the pharmacy.
- Because you are having sedation, you cannot drive and you must have someone accompany you and drive you home.
- You must fast for 6 hours before the appointment (no food at all, including soft drinks, tea and coffee, milk). You may drink sips of water (only) up until 2 hours prior to your appointment.
- You should not smoke for 6 hours prior to the appointment
- If you only require a removal of an IUD, make sure you can feel the string. If you cannot feel the string, please see your GP as you may need an ultrasound beforehand to assess location and position of the IUD.
- If you have any potential of uterine pathology, eg. fibroids, post-menopausal bleeding, etc, you must see your GP first. Prior testing with ultrasound, etc, may be necessary before insertion of an IUD.
- It’s important to not put anything in the vagina for 2 days after insertion (eg. no intercourse, no tampons, no swimming, no baths).
- A follow-up appointment with your GP is recommended 6 weeks after insertion. If any concerns during that time, please contact GCA directly.
Personalised Care and Expertise
Gynaecology Centres Australia believes in providing personalised care and expertise to our patients. Our team of experienced healthcare professionals will guide you through the process, answering any questions or concerns you may have about various Hormonal and Non Hormonal IUD’s. We will discuss your medical history, contraceptive needs, and help you determine which IUD is the right choice for you.


